
Natural ACP Therapy for Osteoarthritis
How the Body’s Own Bioactive Agents Can Help Against Pain
Over 5 million people in Germany suffer from osteoarthritis. Today, the primary focus is on finding treatment methods that can counteract the progression of cartilage degradation and relieve pain. This is exactly where ACP therapy for osteoarthritis comes into its own.
Official Health Partner

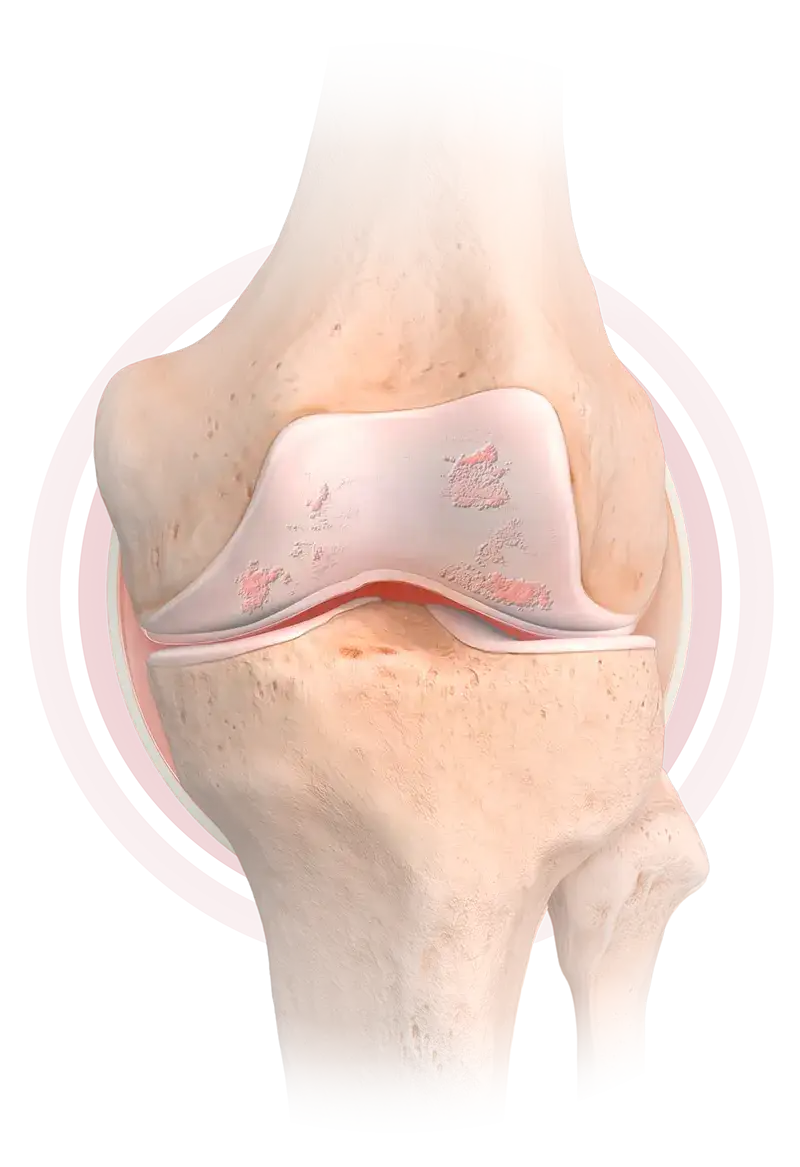
Osteoarthritis is joint wear and tear that is associated with damage to the cartilage. The protective coating on joints gradually wears down, so that in the long-term, adjacent structures such as bones, joint spaces, tendons, ligaments, and muscles can be affected.
Pain Can Limit Quality of Life
Osteoarthritis causes around 2 million people in Germany to suffer joint pain every day, with hands, knees, and hips being most commonly affected. But osteoarthritis can also occur in the shoulders and elbows as well as in the spine.

Osteoarthritis is usually very stressful for patients: joints are painful, mobility is restricted, and quality of life deteriorates. Osteoarthritis cannot be completely cured. But symptoms can be significantly relieved through lifestyle changes and novel treatment methods.
Causes and Symptoms of Osteoarthritis
Causes
Around half of all osteoarthritis patients probably suffer from osteoarthritis due to heavy strain on the joints long-term–through physical work, competitive sports, or obesity, for example. Around a third develop osteoarthritis as a later consequence of injuries such as meniscus damage or cruciate ligament injuries; for the remaining 20%, the cause is weak or deformed joints such as bow legs or knock knees, which can become noticeable at a young age.
physical work
competitive sport
obesity
meniscus damage and cruciate ligament injury
weak or deformed joints
such as bow legs or knock knees
Symptoms
The primary symptoms of osteoarthritis are pain and stiffness in the joints. The symptoms usually get worse with physical exercise, and in damp or cold weather. Affected joints are often stiff for the first half hour after getting up. With start-up pain, pain occurs during movement after rest, but this pain subsides with increasing movement. Doctors make a distinction between different stages of osteoarthritis depending on the progression of the disease.
joint stiffness (after getting up)
gets worse with physical exercise, and in damp or cold weather.
start-up pain
Trust in the Body's Own Strength
ACP Therapy for Arthritis
One treatment option for osteoarthritis is ACP therapy (autologous conditioned plasma therapy). ACP therapy can promote cell regeneration in mild to moderate osteoarthritis (grades I to III) through the body's own natural bioactive agents, such as blood platelets and growth factors.1–3 ACP therapy for osteoarthritis can relieve pain naturally and promote the growth of cartilage tissue, so the balance between cartilage disintegration and growth is largely restored and mobility is also improved. Applications for ACP therapy in osteoarthritis include:




Knee Arthritis
(also knee joint arthritis or gonarthrosis)
Knee osteoarthritis is a slowly progressive, degenerative disease of the knee joint, characterized by wear and tear of cartilage in the knee joint. This condition occurs mainly in older people or following knee joint injuries such as meniscus damage or cruciate ligament tears and can cause pain and restricted mobility. Besides age and injury, the main causes of knee arthritis are obesity, heavy physical work, and sports that place strain on the joints, but also too little exercise and genetic predisposition.
Hip osteoarthritis
(coxarthrosis)
Hip osteoarthritis is a degenerative disease of the hip joint, characterized by wear and tear of cartilage in the hip joint. This leads to pain when walking, stiffness, and difficulty in everyday movement. Hip osteoarthritis is characterized by a narrow joint space in the hip joint due to there being less cartilage, which leads to friction on the bones. It mainly affects people over 50, but besides age, risk factors for hip osteoarthritis include stress caused by heavy lifting, obesity, competitive sports, accidents, and pelvic tilt.
Shoulder arthritis
(omarthrosis)
Shoulder arthritis refers to the degradation of cartilage in the shoulder joint, which is mainly caused by wear and tear, accidents, and disease. For example, bone fractures in the shoulder area or a dislocated shoulder can cause shoulder osteoarthritis. In the advanced stage, pain and restricted shoulder movement are often observed.
Ankle osteoarthritis
(tibiotalar joint osteoarthritis)
Ankle osteoarthritis refers to wear and tear of the cartilage in the upper ankle joint and comes not so much from patient aging, but rather from previous injuries, postural deformity from chronic over-use, rheumatic disease, and obesity. With ankle osteoarthritis, those affected often suffer start-up pain or pain when applying pressure, as well as swelling around the upper ankle joint, which can lead to restricted mobility and even stiff joints over time.
Spinal Osteoarthritis
(also facet syndrome or spondylitis)
Spinal osteoarthritis affects the facet joints, which are the small vertebral joints in the spine, and leads to wear on the joints between vertebrae. Primary causes are applying too much strain or applying it incorrectly, obesity, weak back muscles, family predisposition, and conditions such as rheumatism or osteoporosis. Spinal osteoarthritis typically occurs in old age and leads to back pain in the lumbar spine area and restricted mobility, especially when bending over.
Finger osteoarthritis
Finger osteoarthritis is a degenerative joint condition in which the cartilage layer in the metacarpophalangeal joints of the fingers breaks down, leading to pain, stiffness, and limited mobility. Primary causes are repeated strain on the hands and fingers, genetic predisposition, and aging. Women are affected more often than men, especially after the age of 40.
Elbow osteoarthritis
Elbow osteoarthritis is a degenerative joint condition characterized by the disintegration of cartilage tissue in the elbow joint, which can lead to pain, swelling, and restricted movement. Primary causes are excessive strain, injuries, and aging. Men and women are affected equally, especially in older age or in people who perform repetitive movements.
How Patients Can Actively Support ACP Therapy for Osteoarthritis

Losing weight

Physical therapy

Orthopedic aids such as a walking stick

Moderate exercise such as swimming or cycling
The active cooperation of the patient is also crucial for the success of ACP therapy in osteoarthritis. The aim is to relieve the affected joints and protect them from incorrect or excessive strain, as this alone helps to reduce pain. Using Find a Doctor on our website, you can also find suitable doctors in your area for ACP therapy for osteoarthritis.

How Do Health Insurance Companies View ACP Therapy for Osteoarthritis?
Private health insurance companies often recognize the success of ACP therapy in osteoarthritis and reimburse the costs once ACP treatment is complete. If you have any further questions about ACP therapy for osteoarthritis, please contact a specialist in your area.
Expert opinions and patient reports on ACP therapy for osteoarthritis
“
I noticed that the joint was less swollen and I could put more weight on my right leg again. After a 4-week break from training, I gradually started playing squash again. And the pain relief continued! I go to see Dr. Styra every 2 or 3 months and get a booster. Obviously, there are much nicer things than an injection in the knee. And also much worse!
Knee arthritis patient with Dr. Frank Styra in Munich
“
In practice, 3 to 6 injections within a week have proven effective, depending on the size of the joint. After that, we recommend topping up the biologic therapy every 3 months. The effects can be felt after about 2 weeks.
Dr. Frank Styra, Munich
How Does ACP Therapy Compare to Other Treatment Methods for Osteoarthritis?
Compared to conservative methods such as painkillers, pharmacological infiltration treatments with corticosteroids, hyaluronic acid injections, or surgery, ACP therapy in osteoarthritis represents a natural treatment method that is easy to perform, with few side effects. Thanks to the use of the body's own bioactive agents, intolerances and allergic reactions are avoided and, unlike with drug therapies, the treatment can be repeated as often as desired.
ACP therapy for osteoarthritis not only also has an anti-inflammatory and analgesic effect, it also stimulates the body's self-healing properties naturally, which improves the chances of regeneration over the long term. In combination with other measures such as physical therapy, losing weight, or moderate exercise such as swimming or cycling, ACP therapy is an effective, minimally invasive, and uncomplicated method for treating osteoarthritis.
natural
easy to perform
no side effects
can be repeated as often as desired
anti-inflammatory
analgesic
natural stimulation of the body's own self-healing properties
minimally invasive
ACP Therapy Frequently Asked Questions (FAQs)


How can I actively support ACP therapy for osteoarthritis?
You can support your body in self-healing by doing the following:
- losing weight
- physical therapy
- using orthopedic aids such as walking sticks
- taking moderate exercise such as swimming, or cycling


What is osteoarthritis?
Osteoarthritis is a degenerative joint condition and refers to wear and tear of the cartilage in the joints beyond what is consistent with age.
A host of scientific studies have demonstrated the effectiveness of therapy using the body's own blood in the treatment of various conditions and injuries, especially osteoarthritis, sports injuries, and back pain, establishing it as a very effective and natural alternative to conventional treatment methods.
1
.
Smith PA
;
The American Journal of Sports Medicine
;
Intra-articular Autologous Conditioned Plasma Injections Provide Safe and Efficacious Treatment for Knee Osteoarthritis
;
2016 Apr
;
2016 Apr;44(4):884-91
;
10.1177/0363546515624678;
26831629;
;
Epub
;
1
.
Cerza F et al
;
The American Journal of Sports Medicine
;
Comparison between hyaluronic acid and platelet-rich plasma, intra-articular infiltration in the treatment of gonarthrosis
;
2012 Dec
;
2012 Dec;40(12):2822-7
;
10.1177/0363546512461902;
23104611;
;
Epub
;
1
.
Cole BJ et a
;
The American Journal of Sports Medicine
;
Hyaluronic Acid Versus Platelet-Rich Plasma: A Prospective, Double-Blind Randomized Controlled Trial Comparing Clinical Outcomes and Effects on Intra-articular Biology for the Treatment of Knee Osteoarthritis
;
2017 Feb
;
2017 Feb;45(2):339-346
;
10.1177/0363546516665809;
28146403;
;
Epub
;
